By: Maria Hernandez, Ph.D.
If you’ve been tracking the nation’s progress in the fight against Covid-19, physicians and public health officials of color have been highlighting the need for health equity in the national dialogue. As the data on mortality rates becomes clearer, there is no mistake that the pandemic is impacting African American and Latino communities to a much greater extent. Current mortality rates for Blacks and Latinos is almost 2.8 times that of whites suggesting significant health inequities exist. The discussion about why these inequities are taking place has been less clear and even less clear is how to address this reality.
The key may be in educating healthcare providers about the root cause of these inequities and empowering patients that access healthcare systems.
Health inequities are the differences in health outcomes due to unfair conditions or factors that different populations may face. These factors can include access to quality care, inadequate housing, lack of access to quality food, poverty and systemic racism. Public health researchers and healthcare providers have known about health inequities in the US for over 40 years and the research about what to do point to a confluence of factors that center on economic, educational and social change. Even before the pandemic, Native American and Black women are 2.5 times more likely to die in childbirth than Whites. Women are under diagnosed for heart disease.
Research points to the presence of unconscious and systemic bias as well as a lack of culturally competent care.
https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-andThe pandemic exacerbated the impact of these factors in profound ways. If we look at the fact that essential front line workers–cashiers, bus drivers, food service providers, healthcare workers, postal carriers, warehouse workers, receptionists–have high concentrations of Black and Latino workers, it becomes much easier to understand why so many victims of Covid-19 are from these communities. And if we also explore the role poverty plays in the pandemic, we know that crowded housing conditions where social distancing is not possible has been a factor. The reality is that low income, hourly workers are not able to do their jobs remotely using telecommuting or video conferencing. Many of these workers also experience a harder time finding personal protective equipment that can be a burden for tight household budgets.
The pandemic has set the stage for profound changes in healthcare and its about time.
Two important responses that have emerged in the nation’s healthcare systems is an awareness that physicians, nurses and other caretakers must accept that–like all other human beings–they suffer from unconscious biases. It’s those snap judgements about a person’s race, ethnicity, age, ability, and socioeconomic status that enter into each encounter which can influence the recommended course of care. Those biases can be positive or negative but we all make those associations. The pandemic has accelerated the
extent to which hospitals are seeking training for front line staff and providers in order to reduce the likelihood of these biases and provide more culturally competent care.
These programs include an awareness of how bias impacts the experiences of patients and what may be important factors to consider in working with different populations. Culturally competent care encourages staff to look at how the patient may be experiencing their illness and what their own understanding of how to improve their health. It means taking into account the patients cultural of reference and listening to their unique needs.
Another response is the effort hospitals are making to partner with community clinics, faith based organizations and community organizations to win the trust of patients. This was present before the pandemic, but it has taken on a new sense of urgency as vaccine adoption rates have faltered in Black and Brown communities. Since the implementation of the Affordable Care Act, not for profit hospitals which are the majority of facilities in the US have been asked to report what community benefits they provide to address known community needs.
Despite all of these approaches for improved healthcare services for diverse patients, it will take years before all health systems are aligned on their approach to advance health equity.
The most vulnerable patients need quality care now.
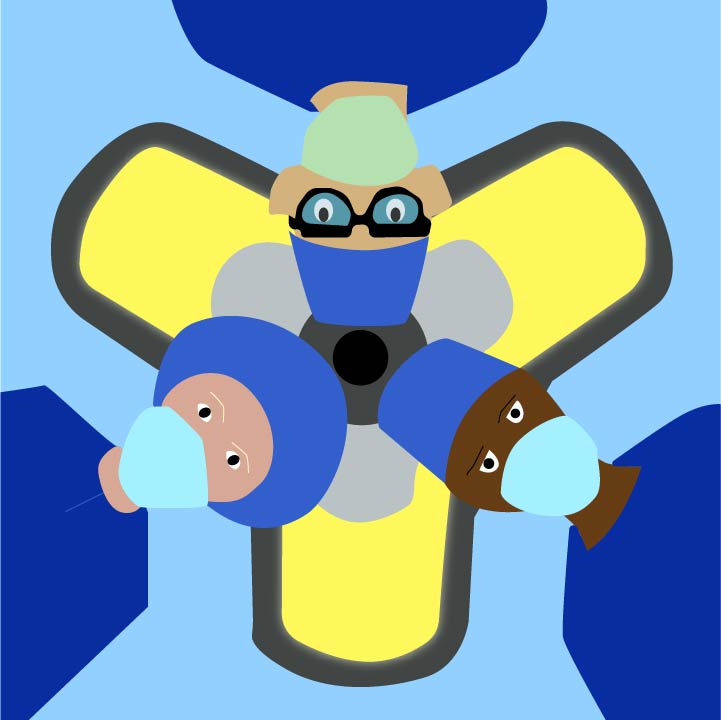
A visit to the doctor—even on-line—may require some key steps to ensure the best care is made available. Three steps that can make a big difference for patient visits. First, bring an advocate with you–a family member or friend who will join you in your visit and support your being heard or to help you ask the right questions. You’ll have to give them permission to be with you given privacy rules in healthcare but it’s worth it. Having a trusted advocate can be a big relief if there’s a lot of options to explore or if there’s different treatment steps involved. There’s a growing field of professional Patient Advocates — sometimes called Patient Navigators that help individuals with navigating treatment options, getting insurance payments, and arranging for home health care if needed. Your health may rely on having someone who understands the complexity of healthcare systems to support you.
Next, review the information your physician provides about the condition or illness and the medicines you may be asked to take. Ask your doctor what information you most need to understand for your treatment or what to do to support your health. Most physicians will provide information on a condition or point you to a reputable website for more information like the Mayo Clinic Review what your physician provides to be informed about the options and treatments presented.
Last, communicate with your care team throughout the course of your treatment or care. If you are struggling with side effects in your treatment or symptoms worsen, call your doctor or the nurse practitioner assigned to your care. Take an active role–with your advocate–to look at options for continued treatment. Poor communication with your physician can put you at greater risk for poor health outcomes. During these challenging days, preparing for each time you visit your physician can set the stage for you to receive the very best care available
About the author -Maria Hernandez, Ph.D., President and COO of Impact4Health is a thought leader in health equity and pay for success initiatives designed to address the upstream social determinants of health among vulnerable populations. Maria currently leads the Alameda County Pay for Success Asthma Initiative which is testing the feasibility of reducing asthma-related emergencies using health education and proven home-based environmental interventions for children.