A career in healthcare is an exciting endeavor that comes with diverse experiences and the ability to positively impact people’s lives.


A career in healthcare is an exciting endeavor that comes with diverse experiences and the ability to positively impact people’s lives.

Taking medication is not without risks, especially for the elderly.

Hailing from Los Angeles, California, brothers, Jake & Papa, bring new heat to the R&B scene. The duo recently released their tracks, “Patient” and “Baby Momma” across streaming platforms. Over the years, the boys have enjoyed regional success with uptempo R&B anthems that can be heard on radio stations across Southern California. “Patient” was discovered […]

MONICA MARTIN RELEASES NEW SINGLE “PATIENT” LISTEN HERE “(Monica Martin) examines the cruelty of denial and staying in a broken relationship.” – NPR [Of “Thoughtless”] “a low-key and ultra-cool track” – NYLON “She is definitely One To Watch.” – Idolator “Martin is both evocative and sinfully infectious to listen to.” – EARMILK “[“Cruel” is] a […]
The 5 Biggest Disruptors As 2019 dawns, some people are taking a “new year-new you” approach. They’re determined to make self-improvements that provide a fresh, positive outlook and strong sense of well-being. But sometimes health factors undermine those good intentions, such as depression and its link to hormone imbalances. There are myriad ways both men […]

Multiple sclerosis, known as MS, is an unpredictable and often disabling disease that disrupts the flow of information between the brain and body. According to the National MS Society, more than 2.3 million people are affected by MS worldwide. Celeste Miranda, CEO and founder of CBD Expo Tour and MACE Media Group, was diagnosed at […]

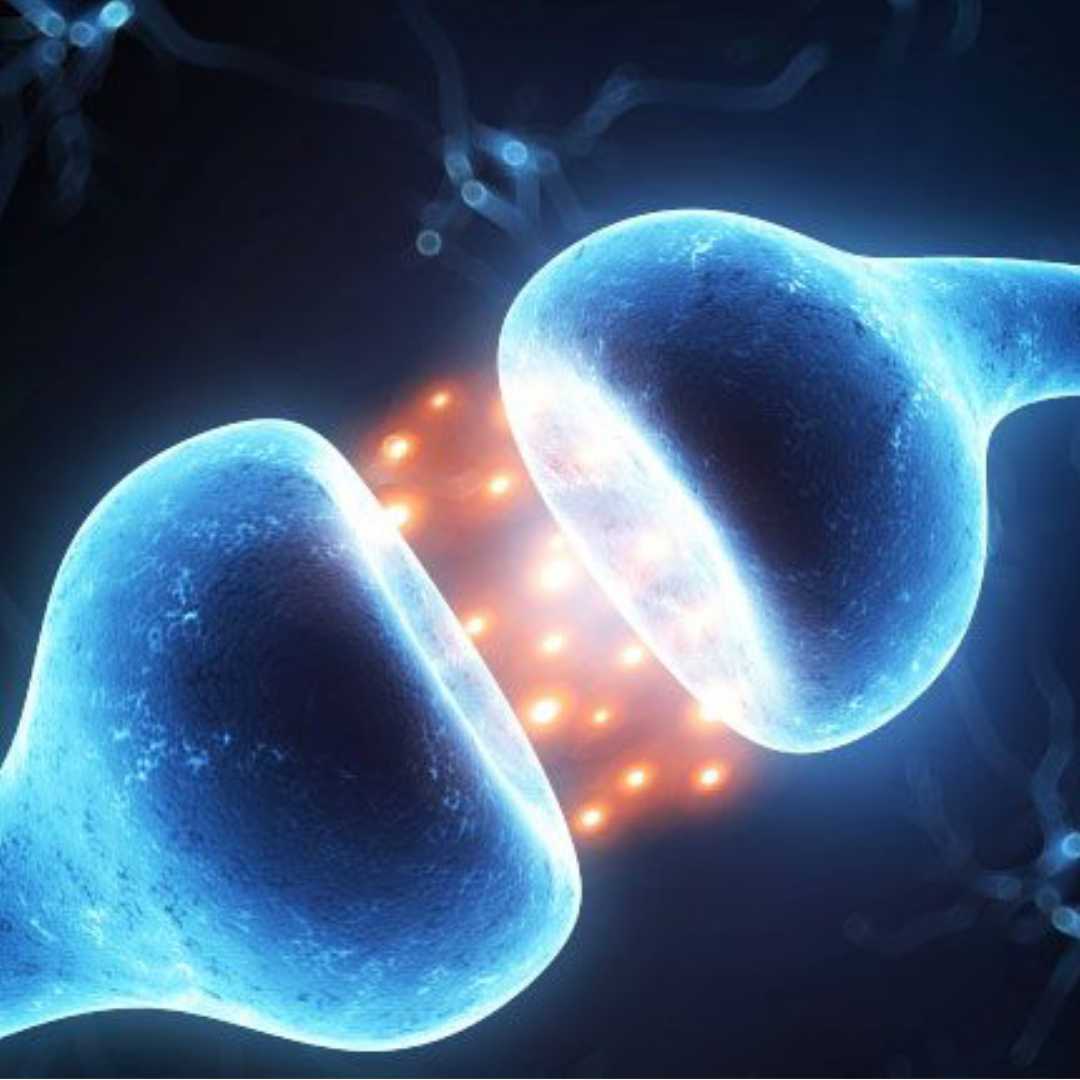
A new study recently published in STEM CELLS Translational Medicine demonstrates the long-term safety of laboratory-expanded endothelial progenitor cells for treating ischemic stroke. This could be good news for the 15 million people who, according to to the World Stroke Organization, suffer from this dangerous condition each year. Ischemic stroke is the most common type […]

In 2009, then Governor of California Arnold Schwarzenegger signed the Donda West Plastic Surgery Law, requiring health checks be conducted prior to all major plastic surgery procedures in the state. This was following the death of rapper Kanye West’s mother. It was later determined that her heart attack was spawned by a combination of numerous […]

New Survey Shows Women Lacking Information for Informed Healthcare Decisions New findings from a recent survey show that women living with chronic inflammatory or autoimmune disease feel they don’t have enough information to make informed decisions about how to balance pregnancy with disease management. Some women feel they have no choice but to stop treatment […]

New findings from a recent survey show that women living with chronic inflammatory or autoimmune disease feel they don’t have enough information to make informed decisions about how to balance pregnancy with disease management. Some women feel they have no choice but to stop treatment or delay their plans for pregnancy. These women are living […]