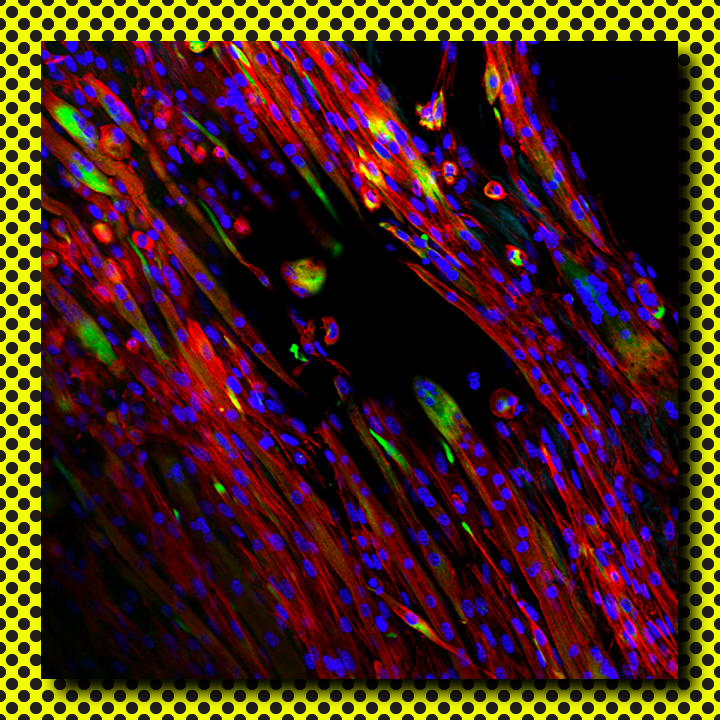
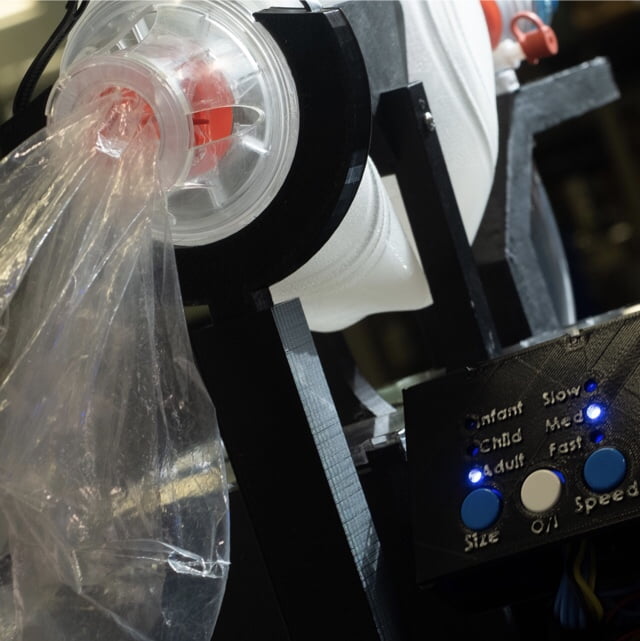
Bio-inspired scaffolds help promote muscle growth Rice University bioengineers adapt extracellular matrix for electrospinning Rice University bioengineers are fabricating and testing tunable electrospun scaffolds completely derived from decellularized skeletal muscle to promote the regeneration of injured skeletal muscle. Their paper in Science Advances shows how natural extracellular matrix can be made to mimic native skeletal muscle and direct the […]