Natalie Dickman squeezed the bag again and again in an effort to revive a victim of cardiac arrest. After a mere 3 minutes, she could squeeze no more.
“The patient had been down for 30 minutes and there wasn’t much hope, unfortunately,” said the Rice University student, a soon-to-be graduate of the Brown School of Engineering, who was covering a shift with Houston EMS as required by a Rice class in emergency medical techniques. “I was allowed to bag, but they make you switch in EMS settings because they know you won’t be as accurate once you hit that 2-to-3-minute mark. You get really tired.”
She thought about that often over the last year when she and her senior teammates worked at Rice’s Oshman Engineering Design Kitchen (OEDK) to perfect a cost-effective device that automates the compression of manual bag valve masks, which feed fresh air to the lungs of intubated patients.
The senior capstone design team — bioengineering students Dickman, Carolina De Santiago, Karen Vasquez Ruiz and Aravind Sundaramraj, mechanical engineering and computational and applied mathematics student Tim Nonet and mechanical engineering student Madison Nasteff — is known as “Take a Breather.”
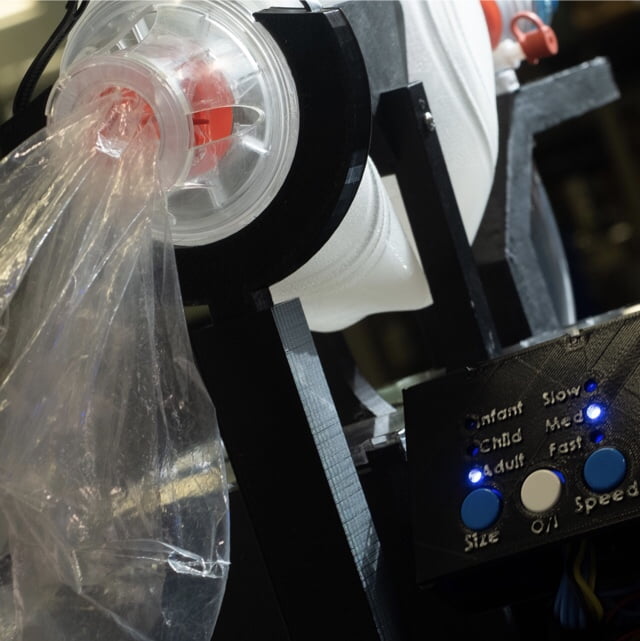
The team has developed a system that compresses the bags for hours, rather than minutes, with settings to feed the right amount of air to adults, children and infants. The device seems simple — a box with paddles that rhythmically squeeze the bulb a programmed amount – but the engineering behind it is not.
The students used a $25, off-the-shelf motor and $5 microcontroller to power and program the rack-and-pinion device made primarily of plastic parts 3D-printed at the OEDK. They hope their use of inexpensive materials and the growing availability of 3D printers will make their machines easy to repair on-site.
They anticipate the device, which cost them $117 in parts to build, will be most useful in low-resource hospitals or during emergencies when there aren’t enough portable ventilators to meet the need.
Dr. Rohith Malya, an assistant professor of emergency medicine at Baylor College of Medicine, brought the problem to the OEDK after witnessing family members at the Kwai River Christian Hospital in Thailand, where he is director of emergency medical services, squeezing intubation bags for hours on end to keep loved ones alive.
“There is no reliable ventilation,” said Malya, who spends a month at the hospital every year. “Once we intubate somebody, the family has to bag the patient. But the family will get tired after a day and say, ‘They’re not getting better right now, just pull the tube and see what happens.’ And then the patient dies.”
Malya previously worked with Rice engineering students to develop a syringe regulating pump, and did not hesitate to bring a new idea to the OEDK.
“The bag mask is ubiquitous, like the syringe,” he said. “Nothing has challenged it for 80 years. It’s stood the test of time, it’s reliable and it’s simple. And now we’re adding a modification to the original device so families don’t have to make those decisions.
“This will broaden the access to mechanical ventilation to a tremendous part of the world that doesn’t have typical ventilators,” said Malya, who plans to take the proof-of-concept device to Thailand for field testing next spring.
The device is much smaller than the sophisticated ventilators found in American hospitals and portable versions used in emergency situations. Critically, it has to be able to operate for long stretches. In its most recent test, the team ran the device for more than 11 hours without human intervention.
The students expect another Rice team will build a more robust version next year, and hope it will eventually be manufactured for use in low-resource and emergency settings. They anticipate a better-sealed and filtered box will be more suitable for hot, dusty environments, and said future designs should include more sophisticated controls.
For its efforts this year, the team won two prizes at the school’s annual Engineering Design Showcase, the Willy Revolution Award for Outstanding Innovation and the best interdisciplinary engineering design award. But the real payoff would be seeing the device further developed and deployed around the world.
“If they can get it working fully in that kind of environment, this will be saving lives,” Nasteff said.